Decontamination
A one system approach to decontamination processes
With the ongoing challenges around managing multiple, disconnected systems, especially when it comes to hospital-wide decontamination processes, a one system approach seems like a no brainer. So why is decontamination still so siloed? And what are the real benefits we can gain from creating one source of truth across the whole Trust?
The Current Challenge: Fragmented Systems
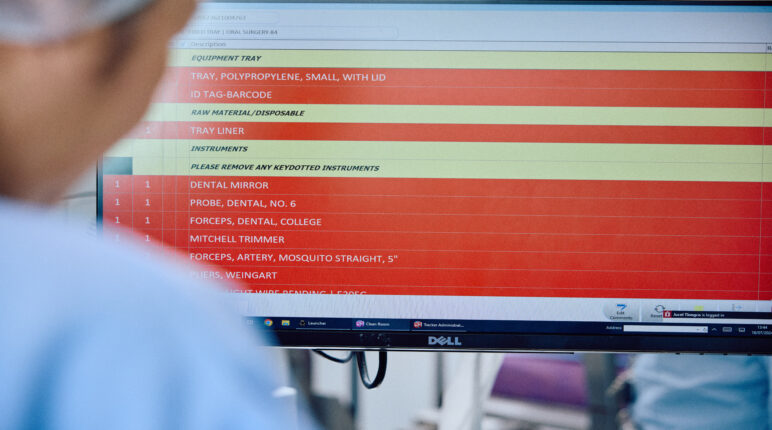
Hospitals often use several different systems across departments such as Sterile Services (SSD), Endoscopy, Gynaecology, and Ultrasound – whether that’s through tech, paper or spreadsheets. These systems may not always communicate with one another. For something as critical as decontaminating medical instruments, this fragmentation introduces inefficiencies and increases the risk of miscommunication or human error. When systems don’t talk to each other, vital information may fall through the cracks, leading to delays, duplication of efforts, or missed steps in the sterilisation processes.
The Case for a One-System Approach
Implementing a one-system approach to manage decontamination processes provides a single source of truth across departments. This enables real-time tracking of instrument sterilisation and usage, making it easier to monitor compliance, streamline operations, and avoid costly errors. A one-system setup ensures:
- Consistency: Standardised procedures across departments, ensuring each instrument undergoes the same stringent sterilisation regardless of where it’s used.
- Visibility: A unified view of decontamination processes that makes it easier to identify inefficiencies or gaps.
- Accountability: A clear chain of responsibility, reducing the chances of errors that might lead to hospital-acquired infections (HAIs), which are not only dangerous for patients but also expensive for hospitals.
How Centralising Decontamination Leads to Savings
1. Reduction of Hospital-Acquired Infections (HAIs)
HAIs remain a costly burden to the NHS. Centralised decontamination processes are more likely to catch sterilisation issues before they result in infection. According to a study, hospitals focusing on reducing variation in care (including consistent decontamination processes) saw a substantial reduction in infection rates, leading to lower treatment costs. Preventing even a small percentage of HAIs can translate into significant savings. Each avoided infection reduces treatment costs and bed days required for affected patients.
2. Optimising Resource Allocation
One system helps manage inventory more effectively by tracking the real-time status of instruments. This reduces unnecessary spending on replacement instruments or outsourcing sterilisation services. You know precisely where each piece of equipment is, whether it’s been sterilised, and if it’s ready for use. This reduces redundancy and the need to keep more expensive instruments than you need.
3. Improved Workflow Efficiency
Using disconnected systems often results in redundant steps or delays in instrument availability. This fragmentation slows down procedures, leading to inefficiencies in staff productivity and surgery schedules. A single system improves workflow by reducing the time spent searching for available, sterile instruments or waiting for sterilisation updates from different departments. Faster turnaround times lead to more efficient use of operating rooms, reducing costs associated with delays.
4. Data-Driven Decision-Making
A centralised system provides important data on decontamination processes, enabling hospitals to make more informed decisions about where to invest resources. For example, it can help identify bottlenecks in workflows, helping teams adjust. Hospitals that use data from one unified system to guide decisions have reported significant financial savings, as they can better manage equipment, staff allocation, and patient flow.
5. Reduced Administrative Burden
Managing multiple digital systems increases administrative complexity and costs. Multiple systems also means multiple contracts, invoices and costs. Staff then need to input data into different systems, increasing the chance of errors and prolonging administrative tasks. By using one system, hospitals can reduce time spent on manual data entry, lower the chances of input errors, and minimise the need for extensive system training for staff.
In summary…
A one-system approach to decontamination is not just about compliance; it is an opportunity to create real financial savings. By improving efficiency, reducing HAIs, and lowering administrative burdens, hospitals can allocate resources more effectively and reduce operational costs. In a time where healthcare budgets are under immense pressure, streamlining these processes can help free up funds to improve patient care.
Switching to a centralised decontamination system is not just a technical upgrade, but a strategic decision that can save hospitals significant money and improve care quality. It’s time to stop managing sterilisation in silos and start benefiting from a more unified, efficient approach.
Book a Demo
Arrange a one-to-one demonstration with a member of our dedicated team. We collaborate to tailor the experience so you can see how our solutions can be applied in your specific context and utilised effectively to achieve your objectives.