Clinical outcomes
Clinical Safety
NHS
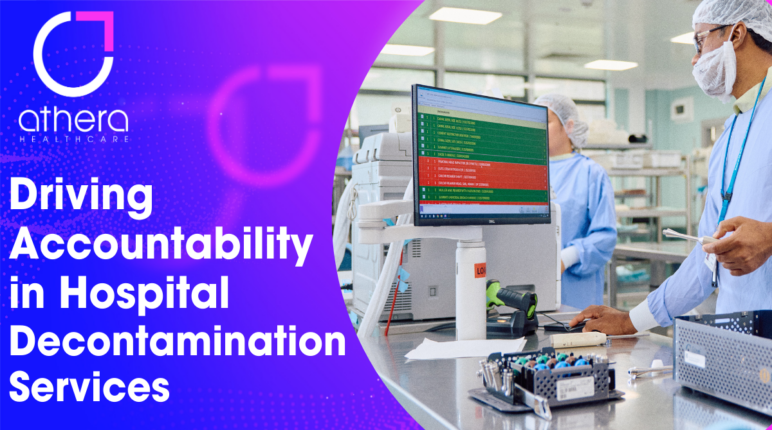
Driving Accountability in Hospital Decontamination: The Role of Data in Improving Quality Management
Earlier this year, the NHS released an updated competency framework that emphasises the need for stronger board-level oversight, governance and accountability in sterile services and decontamination departments.
This focus on governance is essential to improving patient safety and reducing healthcare-associated infections (HCAIs), which affect 300,000 patients annually in the NHS. In response, hospitals are being urged to move away from reactive approaches and instead adopt data-driven systems to monitor, predict, and manage the quality of their sterile services.
But what does this shift mean for hospital leadership, and how can the right technology help drive these changes? Let’s look at why the NHS’s latest recommendations are so important and how healthcare leaders can meet these new standards by embracing data as a tool for accountability.
The Need for Stronger Oversight in Decontamination
Decontamination and sterilisation services play a critical role in ensuring the safety of surgical equipment and preventing infection. However, the processes in these departments are often hidden to hospital leadership, with the risk of quality issues not being identified until it’s too late.
The NHS’s push for board-level oversight recognises that sterilisation departments must no longer operate in isolation. They need to be part of a hospital-wide system of governance where standards are monitored in real-time, and issues are addressed before they can escalate.
Without a structured system of accountability, inconsistent sterilisation processes can lead to equipment malfunctions, surgery delays, and, ultimately, a higher risk of infections. Infections acquired during hospital stays, are not only dangerous but also costly, with the NHS estimating a financial burden of over £1 billion each year.
Moving from Reactive to Predictive Management
Historically, SSDs have relied on reactive maintenance and manual oversight. This means issues are often only addressed after they’ve caused a problem, such as a delayed surgery due to faulty equipment or a breach in sterilisation protocol. This reactive approach can no longer meet the growing demands of healthcare, where every delay and failure can impact patient outcomes.
To address this, hospitals need to adopt predictive tools that can identify potential problems before they happen. With the right data, hospitals can monitor machine performance, track compliance with sterilisation protocols, and identify any emerging trends that suggest a problem may occur.
This predictive management is exactly what the NHS is pushing for with its focus on board-level oversight. It’s about giving hospital leadership the visibility and data they need to ensure that decontamination services are running smoothly, efficiently, and safely.
How Data Enhances Accountability
Here at Athera, we understand the importance of data in driving accountability, especially in sterile services. That’s why we developed Fingerprint, a solution designed to provide hospitals with the data and insights they need to improve decontamination processes.
How can FingerPrint help your team?
- Real-time data tracking: Fingerprint allows hospitals to track every instrument from the moment it enters the sterilisation process to when it’s used in surgery. This level of detail ensures that no step in the process is missed.
- Predictive maintenance alerts: Rather than waiting for equipment to break down, Fingerprint uses data to identify when machines need maintenance or calibration. This helps prevent costly delays and potential contamination risks.
- Compliance monitoring: Fingerprint tracks compliance with sterilisation protocols, alerting teams if any steps are skipped or if equipment hasn’t been properly processed.
- Customised reporting: Hospital leadership can access real-time reports and analytics that provide a clear picture of how well decontamination services are performing, enabling quicker decision-making.
This type of data-driven approach means hospitals can respond to issues faster, improve the efficiency of their sterilisation departments, and reduce the likelihood of infections spreading through improperly cleaned equipment.
A Shift to Proactive Leadership
The NHS’s call for increased board-level oversight is about more than just improving processes; it’s about creating a culture of proactive leadership where hospital boards have the information they need to make strategic decisions.
For hospital leaders, this means moving beyond reactive systems that only show when things go wrong. Instead, they need access to data that highlights potential risks, measures performance in real time, and ensures that high standards are maintained consistently across the board.
The benefits of this shift are clear:
- Reduced infection rates: With more reliable decontamination processes, hospitals can significantly lower their rates of HCAIs, leading to better patient outcomes.
- Operational efficiency: Data-driven tools allow hospitals to optimise their sterilisation schedules and workflows, reducing unnecessary downtime and avoiding surgery delays caused by equipment failures.
- Cost savings: Preventing infections and avoiding delays can save hospitals substantial amounts of money. With HCAIs costing the NHS around £1 billion annually, any reduction in infection rates represents a significant financial benefit.
Data as a Tool for Change
Data is the key to this transformation. Without it, hospital boards are left guessing about what’s happening in their decontamination departments. With the right data, however, they can see exactly what’s working, what needs improvement, and what steps to take to fix issues before they impact patients.
At Athera Healthcare, we believe that data should be at the heart of every decision hospitals make, especially when it comes to critical services like sterilisation and decontamination. Fingerprint is designed to give you the insights you need to drive accountability, improve patient safety, and meet the NHS’s latest recommendations.
By bringing decontamination reporting into the data-led era, hospitals can not only meet the new standards for oversight and governance but also create a safer, more efficient environment for both staff and patients.
A future built on accountability and intelligence
The NHS’s April 2024 bulletin sets a clear mandate for hospitals: stronger board-level oversight and greater accountability are needed in decontamination and sterile services. Adopting data-driven solutions like Athera Fingerprint allows hospitals to shift from reactive to predictive management, ensuring that decontamination processes are not only compliant but optimised for performance.
Book a Demo
Arrange a one-to-one demonstration with a member of our dedicated team. We collaborate to tailor the experience so you can see how our solutions can be applied in your specific context and utilised effectively to achieve your objectives.